COVID Cases Are Rising—and So Are New Treatments

"You still should be wearing a mask, washing your hands, all the basics. Don’t let up. If you’re elderly, sick, have health problems, you should err on the side of sheltering in place," Dr. Voelker says.
Image: Shutterstock by Drazen Zigic
Florida surpassed 100,000 cases of the coronavirus this week, and a record-breaking 5,508 new cases were reported on Wednesday, June 24, alarming public health experts here and around the country. At the beginning of June, Florida’s positivity rate (the daily rate of positive cases relative to the daily number of people tested) was 4 percent. On Monday, it was 10.89 percent.
Sarasota County has had a total of 1,091 cases, with 95 deaths and a 3.4 percent positivity rate. Sixty new cases were reported today. Manatee County has had a total of 2,132 cases, 127 deaths and has a 6.5 percent positivity rate.
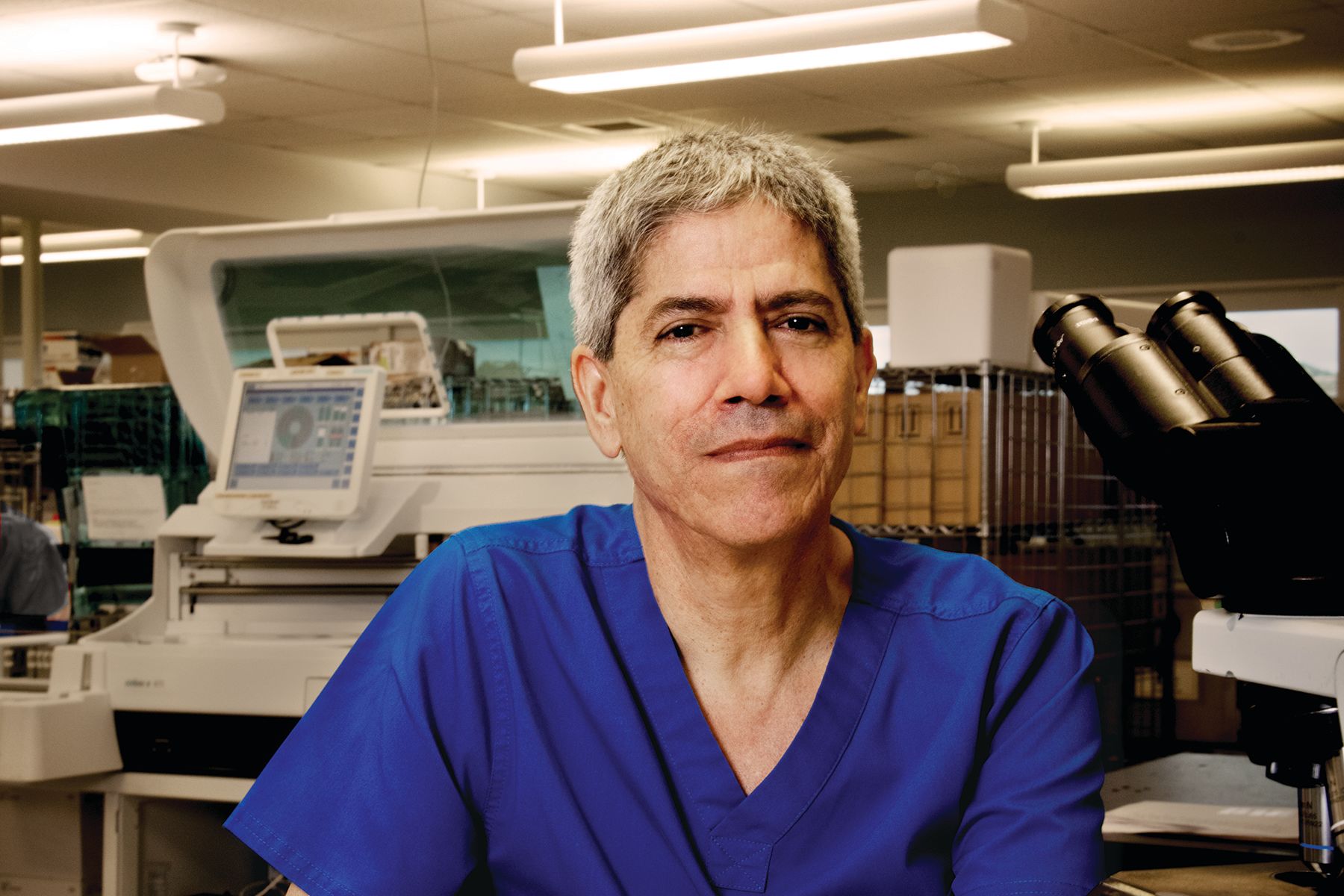
We talked to Dr. Kirk Voelker, a Sarasota pulmonary critical care and ICU physician and the medical director of clinical research at Sarasota Memorial Hospital, about the increase in cases and the new promising treatments to fight the disease. Starting last week, Voelker said doctors have five ways to battle COVID-19 that they didn’t have when they began seeing cases in March.
“We were excited a couple of weeks ago when the ICUs emptied out and there were no COVID patients but, unfortunately, that’s not the case now. It’s concerning. [Last] week we started to see an increase. We went from zero patients to five. [Editor’s note: It was six on Monday.] We had a death a couple of days ago. Deaths are a lagging indicator, meaning that people will be very sick for three, four weeks before they finally succumb.
“Initially when this whole thing started out, we were in touch with critical care physicians in Seattle, New York, New Orleans—getting their experience. And we were basing our treatments on their experience. And it was all in real time and it would change sometimes day to day. We have learned so much and it’s all been on the fly. There was no rule book and we didn’t have any tools to fight it. But now we have a better handle on it.
“Being outside, at the beach, your chances of catching or giving COVID to someone are extremely low. What we’re learning about COVID is that it takes prolonged exposure to somebody who has it, 15 minutes or more. If you’re walking by somebody at the beach, you’re not going to catch it. I would encourage people to start exercising, start walking. Don’t be afraid to go out. if you’re outside walking around in the open air, you’re probably not transmitting walking by people. But when you’re going to join other people, have your wits about you. Follow CDC recommendations. You still should be wearing a mask, washing your hands, all the basics. Don’t let up. If you’re elderly, sick, have health problems, you should err on the side of sheltering in place.
“We started out with hydroxychloroquine because it had a theoretical benefit, then found out that it wasn’t a benefit and that it may have prevented one of the other drugs, Remdesivir, from affecting the virus.
“We now have five things we didn’t have at the beginning of this disease. Remdesivir is the antiviral agent. It works against the virus and hinders it from replicating. It’s best used early when people are starting to require oxygen. It’s available only under FDA emergency use. You have to be in the hospital and requiring oxygen.
“The next thing we have is convalescent plasma. Somebody who’s had the disease before creates antibodies. Taking their antibodies and infusing it into somebody who has COVID now can help to fight it. This is still under clinical trial [but] it’s worked in previous coronavirus cases, such as in MERS and SARS. That being said, anecdotally, we sometimes see that when people are running high fevers and their immunity system is going crazy, we can give them the convalescent plasma and things calm down. It’s become one of our mainstays in fighting this.
“Right now, we only have seven more doses of convalescent plasma. Each patient gets one dose, maybe two. And it’s blood-type specific. If we don’t have it in your blood type, you don’t get it. There’s a real need for the Sarasota community to pitch in and help. One person that had COVID can save four more people. And they can donate every 28 days. We can see [improvements] within 12 to 24 hours in these patients. Plasma can be frozen, and we need to stock up for the future.
“We’re also using Tocilizumab. It’s a drug for rheumatoid arthritis and lupus that calms down the inflammation pathway. Part of the problem with the COVID response is that you get this cytokine storm, this inflammation that goes crazy and affects your kidney, your lungs, your liver and your heart, and it’s in part due to this inflammation process. Tocilizumab is not FDA approved for COVID but is approved for other things, so we are using it to calm down that cytokine storm.
"And that brings us to Dexamethazone. This medicine has been around for 50 years. It’s a steroid, and it’s cheap and readily available. [On June 16] they announced a study out of the UK that looked at it in 6,000 patients. For those who received Dexamethazone and were on breathing machines, there was a decrease in mortality of one third. That’s huge. All we have is the initial report, not the final paper, so we can’t scrutinize the data, but it has potential to save lives. It also showed that for people on oxygen, before they get to the ventilator, it decreases mortality by 20 percent. As soon as I looked at the information, I put all of my patients on the ventilator on Dexamethazone. It’s only been two days so it’s hard to say how effective it is. My patients are getting better, but I’m throwing the kitchen sink at them.
“Another thing we have for patients whose kidneys fail and who are on continuous dialysis 24 hours a day, is a new filter that absorbs some of the cytokines and decreases systemic inflammation. COVID affects the kidneys. Three out of my five patients in ICU are on that as well. These are five things we didn’t have at the beginning of this disease.
“The utility of testing for COVID for an individual person is not that great. You can test negative now and then, three days later, get it. Where it is beneficial is that once you get a case report—let’s say you’re in a nursing home—then we know we need to go in and test everybody to see how prevalent it is and to see who’s affected and who’s not affected and test them frequently to prevent spread. It’s a public health benefit.
“You have to take the long view. Initially the question was is this thing going to go away like the flu goes away? Are the interventions working, or does it go away on its own? Did we overreact by shutting everything down? The fact that now as we’re lightening up on our restrictions and we’re seeing a resurgence shows that what we did was working. It’s not going away on its own. It has a long tail. The slope keeps coming down, but it keeps on going, going, going. Now the question is whether it’s going to flare up again or not. I don’t think anybody can really tell you.
"We’re hoping we have a vaccine. But we need to be prepared for another wave in the fall. If it doesn’t happen that’s great, but we have to stockpile plasma."
Editor's Note: SunCoast Blood Centers is testing all blood donors for the antibodies to COVID-19 and is asking anyone who tests positive to donate plasma. This test will be offered through August 31, 2020. The test is authorized by the Food and Drug Administration (FDA) for detecting the presence of antibodies against SARS-Co V-2 and is not intended to diagnose or treat COVID-19. Donors should be well and healthy at the time of donation and must meet all donor criteria. For information about testing call (941) 413-1011 or visit suncoastblood.org.